Inspiring Stories From the MSK Giving Community
Explore powerful stories from the MSK Giving community, where donors make a transformative impact on cancer research, education, and patient care at MSK. Discover how your support can fuel groundbreaking advancements and inspire hope.

MSK Update
December 27, 2025
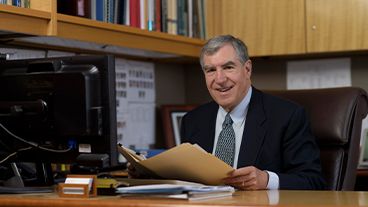
Remembering Louis V. Gerstner, Jr., Longtime MSK Trustee and Champion of Cancer Research

Supporter Story
A Life Remembered Through Philanthropy

Supporter Story
October 8, 2025
Reflecting on the Future: The Gift of Time Inspires a Daughter to Give Back

Supporter Story
FAO Schwarz: Spreading Joy Through Generosity

Supporter Story
June 20, 2025
Expanding Cancer Care Access: A Legacy of Gratitude and Innovation at MSK
Help fuel a future of new firsts
Every day, MSK brings courage and creativity to answering cancer’s biggest questions, and we have set an ambitious goal to create more hope, possibility, and cures for every person with cancer.
All ways to give
As an MSK donor, you can bring hope for new cures to people worldwide. Learn about the many ways you can support MSK’s mission.